Dr Priyadarshi Amit MS DNB MCh FRCS

Gold Medallist in Orthopaedic Surgery
Dual Fellowship Trained Surgeon in the UK
Fellow of Royal College of Surgeons of England
Specialist Shoulder Elbow & Upper Limb Surgeon
Member of British Elbow & Shoulder Society (BESS)
Member of Shoulder & Elbow Society of India (SESI)
Director of Delhi Shoulder Arthroplasty Course (DSAC)
Previous NHS Consultant in York & Scarborough NHS Trust
Division Head Upper Limb Surgery, Amrita Hospital Delhi NCR

Our Services


Wrist surgery is performed to treat a wide variety of conditions, including fractures, carpal tunnel syndrome, arthritis, ligament injuries, ganglion cysts, and more. The goal is to restore function, reduce pain, and improve the patient’s quality of life. Surgery may be minimally invasive (arthroscopic) or open, depending on the condition.
Surgical Process
- Pre-operative Evaluation
- Imaging: X-rays, MRI, or CT scans.
- Physical examination and medical history.
- Blood tests and anaesthesia evaluation.
- Day of Surgery
- Performed under local, regional, or general anaesthesia.
- Duration: Typically 30 minutes to 2 hours.
- Outpatient or short hospital stay.
- Post-operative Care
- Immobilization (splint or cast) for 2–8 weeks.
- Pain management: NSAIDs, ice, sometimes opioids.
- Physical therapy often starts after initial healing.
Recovery Timeline:
- First Week: Swelling, pain, immobilization.
- Weeks 2–6: Stitches removed; slow return of motion with therapy.
- Months 2–6: Regaining strength, full range of motion.
- Beyond 6 Months: Final functional outcomes apparent.
Risks and Complications
| Infection | Especially in open procedures. Rare but serious. |
| Nerve Damage | Potential numbness, tingling, or weakness. |
| Stiffness | Common after immobilization, can persist long-term. |
| Non-union | Especially in bone fusion/fixation surgeries. |
| Implant Failure | In wrist replacements; may need revision. |
| Scar Sensitivity | Especially in carpal tunnel or open surgery. |
Wrist surgery can be life-changing for those suffering from persistent pain or injury. The type of procedure, surgeon’s expertise, and patient adherence to rehab are key to a successful outcome. While it involves downtime and risk, most patients experience significant improvement in function and pain relief.

Hand surgery is a specialized branch of orthopaedic that addresses conditions affecting the hand, wrist, and forearm. These surgeries can range from minor tendon repairs to complex reconstructions involving bones, nerves, and vessels. The goal is to restore function, relieve pain, and improve aesthetic appearance when necessary.
Surgical Experience
- Pre-operative Process
- Patients undergo physical exams, imaging (X-ray, MRI), and may receive a nerve conduction study.
- Informed consent is crucial; risks like infection, stiffness, or nerve damage are discussed.
- Anaesthesia
- Varies by procedure: local, regional (brachial plexus block), or general.
- Outpatient surgeries are common unless extensive work is needed.
- Intraoperative Care
- Surgeons often use a tourniquet and magnification tools.
- Meticulous technique is vital to preserve function.
Recovery and Rehabilitation
- Post-operative Pain
- Usually well-managed with oral pain medications and elevation.
- Pain typically subsides in a few days to a week.
- Splinting/Casting
- Immobilization is common post-op, especially for tendon or bone work.
- Duration ranges from a few days to several weeks depending on the surgery.
- Physical Therapy
- Critical component of recovery.
- May include passive and active range of motion exercises, strength training, and scar management.
- Occupational therapy helps patients regain daily function.
Risks and Complications
- Common risks:
- Infection
- Nerve injury
- Stiffness or reduced range of motion
- Scar sensitivity
- Recurrence of the original condition
- Rare but serious risks:
- Complex regional pain syndrome (CRPS)
- Non-union or malunion of fractures
- Loss of limb viability (in trauma cases)
Hand surgery can be transformative for those suffering from injury, degenerative disease, or congenital abnormalities. While outcomes are typically positive, success heavily depends on:
- Surgeon expertise,
- Timely intervention,
- Commitment to rehabilitation.
It’s not a one-size-fits-all solution, but when approached with proper planning and realistic expectations, hand surgery can significantly improve quality of life.

The shoulder joint is a highly mobile joint between the shoulder blade (also called ‘scapula’) and the arm (also called ‘humerus’). The shoulder joint connects the upper body to the arm. Its function is to allow positioning of the hand enabling it to perform various tasks. It is commonly affected by sports injuries and wear and tear. When affected, it causes pain, restricted movement or instability, which compromises the overall function of the upper limb.
Shoulder surgery is a medical procedure performed to treat injuries, degenerative diseases, or structural issues in the shoulder joint. When conservative treatments like physical therapy, medication, or injections fail, surgery is often the next step. It is usually performed through two approaches :
- Arthroscopic Surgery – During arthroscopic surgery, tiny incisions are made over the shoulder joint through which the camera and other instruments are inserted. These are used to perform repair of the torn tendons or ligaments such as rotator cuff repair or labral repair.
- Open Surgery – Open surgery is performed via long incision over the skin either on the front or side or back of the shoulder. These classically are used for surgical fixation of a fracture or a joint replacement surgery.
Preoperative Considerations
Diagnosis: MRI, CT, and X-rays help confirm the issue.
Non-surgical Options First: Most doctors try physical therapy, cortisone shots, or rest before suggesting surgery.
Prehab: Physical therapy before surgery may improve outcomes.
Informed Consent: Patients must understand risks, expected outcomes, and recovery.
Surgical Procedure
Setting: Usually same-day surgery unless a full replacement is done.
Anesthesia: General or regional (nerve block).
Duration: Typically 1–2 hours.
Postoperative Recovery
- Immediate Aftercare
* Use of a sling for several weeks.
* Pain managed with NSAIDs, opioids (short-term), or nerve blocks.
* Ice and elevation to reduce swelling.
- Rehabilitation
Phase 1 (0–6 weeks): Immobilization with passive movement.
Phase 2 (6–12 weeks): Active-assisted and active motion.
Phase 3 (3–6 months): Strengthening and return to full activity.
- Return to Work/Sport
Desk work: 2–4 weeks.
Manual labor: 4–6 months.
Sports: 4–9 months depending on sport and surgery type.
Benefits
* Pain relief.
* Improved shoulder function and strength.
* Greater range of motion.
* Return to normal activity or sport.
* Slows down degenerative changes in the joint.
Risks and Complications
* Infection.
* Stiffness.
* Nerve or blood vessel damage.
* Failure of repair or need for revision surgery.
* Complications from anesthesia.
* Blood clots (rare in upper extremity procedures).
Patient Experiences
Positive Experiences:
* Many patients report significant pain relief and improved function.
* Athletes often regain pre-injury performance levels.
* Arthroscopic procedures generally result in faster recovery and fewer complications.
Challenging Experiences:
* Long recovery time can be frustrating.
* Physical therapy is often intensive and critical to success.
* Sleep disturbances due to pain are common early on.
* Some elderly patients or those with massive rotator cuff tears may experience only partial improvement.
Shoulder surgery can be highly effective when done for the right reasons, with careful pre-op planning and diligent post-op rehab. While recovery can be lengthy and requires patience, the outcomes are generally favourable, particularly for patients motivated to follow through with therapy.

Elbow joint is hinge joint between the arm bone (humerus) and forearm bones (radius and ulna). It comprises of ulno-humeral joint, radio-capitellar joint, and proximal radio-ulnar joint. It is supported by important ligaments on both sides, lateral collateral ligament and medial collateral ligament.
It is mostly affected by trauma, sports injuries, fractures, tendon tears, nerve compression, and arthritis. When affected, it causes pain and restricted movement of the joint, limiting overall upper limb function. When conservative treatments—like physical therapy, bracing, medication, or injections—fail, surgical intervention may be recommended such as repair of the torn ligaments or tendon, nerve decompression, arthroscopic debridement, fixation of fractures, or elbow replacement.
Preoperative Process
- Imaging: X-rays, MRI, or CT scans to determine the extent of damage.
- Conservative Management First: Physical therapy, NSAIDs, bracing, and steroid injections are usually tried before surgery.
- Informed Consent: Includes risks, benefits, recovery timeline, and realistic expectations.
- Pre-op Physical Therapy: Sometimes recommended to improve baseline function.
The Procedure
- Setting: Most procedures are outpatient unless a major reconstruction or replacement is performed.
- Anaesthesia: General or regional block (brachial plexus block).
- Surgical Duration: Varies—30 minutes (simple arthroscopy) to 2+ hours (replacement or fracture repair).
- Instruments: Arthroscope (minimally invasive), or open surgical tools for more complex repairs.
Postoperative Recovery
- Immediate Recovery
- Splinting or bracing may be required.
- Pain managed with oral medications or regional anaesthesia.
- Ice and elevation help reduce swelling.
- Rehabilitation
- Phase 1 (0–2 weeks): Rest, protect joint, manage pain and swelling.
- Phase 2 (2–6 weeks): Begin gentle range-of-motion exercises.
- Phase 3 (6–12+ weeks): Progressive strengthening and return to function.
- Return to Activity
- Desk work: 1–3 weeks depending on surgery type.
- Manual labour: 3–6 months.
- Sports: 4–9 months (especially throwing sports).
Benefits of Elbow Surgery
- Significant pain relief.
- Improved joint mobility and strength.
- Restored nerve function (in cases of compression).
- Correction of deformity or instability.
- Return to daily activities or athletic performance.
- Prevention of long-term joint degeneration.
Risks and Complications
- Infection.
- Nerve injury (especially ulnar or radial nerve).
- Persistent stiffness or loss of motion.
- Chronic pain or complex regional pain syndrome (CRPS).
- Hardware failure or loosening.
- Blood clots (less common in upper extremity).
- Failure of tendon or ligament repair.
- Need for revision surgery.
Elbow surgery can be life-changing for patients with chronic pain, instability, or injury that limits arm use. While outcomes are generally positive, patient motivation, adherence to rehab, and the experience of the surgeon play crucial roles in success. Not every elbow condition requires surgery, but for those who do, advances in surgical techniques—especially minimally invasive approaches—have significantly improved results and shortened recovery times.

At OSS, we have expertise in the non-operative management of musculoskeletal pain and sports injuries. Surgery will be offered to treat your injury only if considered necessary. Our experts will evaluate your injury, consider necessary investigation, and prescribe the necessary treatment to help you recover from your injuries. We aim to keep you active regardless of your age or level of activity, so that you can enjoy what you love to do.
Common sport injuries we treat
- Joint pain
- Musculoskeletal pain – pain in the bone or muscle or tendon or ligament (sprain or strain)
- Ligament tear such as MCL tear or labral tear
- Tendon tear such as rotator cuff or biceps or triceps or pectoralis major tendon tear
- Tendinitis or tendinopathy
- Exercise induced pain
- Joint dislocations
Facilities
Rehabilitation & Training
At our clinic, the majority of sports related injuries are treated successfully with exercises, enabling a full return to previous levels of activity. After thorough evaluation of your condition, the consultant will offer you exercises to improve your pain. Our consultants will also recommend pre-operative rehabilitation (Prehab) to prepare you physically for surgery when you need.
Ultrasound Guided Injections
To reduce pain and inflammation, our consultants will consider injections into your joint or around the tendons. Common injections given at our clinic are steroid, hyaluronidase, platelet-rich-plasma (PRP) and bone marrow aspirate concentrate (BMAC). Our specialists have the expertise in giving ultrasound-guided injections with greater accuracy and better patient outcome.
Sports surgery
It is a subspecialty of orthopaedic surgery that focuses on the treatment of injuries related to sports and physical activity. These surgeries aim to restore function, reduce pain, and return athletes—both professional and recreational—to their prior level of performance.
Sports surgeons often treat acute injuries (like ligament tears) and chronic conditions (like tendonitis or impingement syndromes) that fail to improve with non-surgical treatment.
Surgical Techniques
- Arthroscopy (minimally invasive)
- Small incisions, faster recovery, less scarring.
- Open Surgery
- Necessary for more complex reconstructions.
- Longer healing time, but may provide better access for certain repairs.
Common Upper Limb Sports Surgeries treated at OSS are
The Surgical Experience
Pre-Operative
- Comprehensive assessment includes physical exam, imaging (MRI, X-ray), and functional testing.
- Athletes are often guided through prehabilitation to strengthen the area before surgery.
Anaesthesia
- General anaesthesia or regional blocks are commonly used, depending on the procedure.
Hospital Stay
- Most sports surgeries are outpatient procedures.
- Patients typically go home the same day with a brace, sling
Recovery and Rehabilitation
- Initial Recovery (0–2 weeks): Pain control, swelling reduction, immobilization.
- Early Rehab (2–6 weeks): Gradual passive and active motion.
- Strengthening Phase (6–16 weeks): Functional strengthening and neuromuscular control.
- Return-to-Sport (4–12 months): Sport-specific drills, performance testing.
Physical Therapy
- A cornerstone of successful recovery.
- Customized programs based on sport, position, and goals.
- May include balance training, endurance, plyometrics, and proprioception.
Outcomes and Return to Play
- Return-to-Sport Rates vary by injury, sport, and level of play.
- Many athletes regain pre-injury levels.
- Some sports show decline in explosiveness or durability depending on the surgery.
Risks and Complications
- Infection
- Blood clots (DVT)
- Stiffness or loss of motion
- Graft failure or re-tear
- Nerve injury (rare)
Psychological Aspects
- Athletes may face fear of re-injury, anxiety about performance, and identity loss.
- Mental readiness is a crucial factor in successful return to sport.
- Many teams incorporate sports psychologists into the rehab process.
Sports surgery is an essential tool in modern athletics, offering athletes a path back to performance after injury. While not all injuries require surgery, when conservative treatment fails, surgical intervention can restore function and extend careers.
Key factors in successful outcomes include:
- Timely and accurate diagnosis,
- Skilled surgical technique,
- Personalized and consistent rehabilitation,
- Strong mental resilience.
Sports surgery is not a shortcut—it’s a strategic reset that, when done properly, can lead to full recovery and even enhanced performance.
Success Stories


Asian Deaf Games 2024

Mr Sumit Dahiya underwent Elbow Arthroscopy Surgery, won Gold Medal in Asian Deaf Games 2024

UKBFF championship 2022

Mr Ivo Eglitis underwent Pectoralis Major Repair, won UKBFF championship 2022
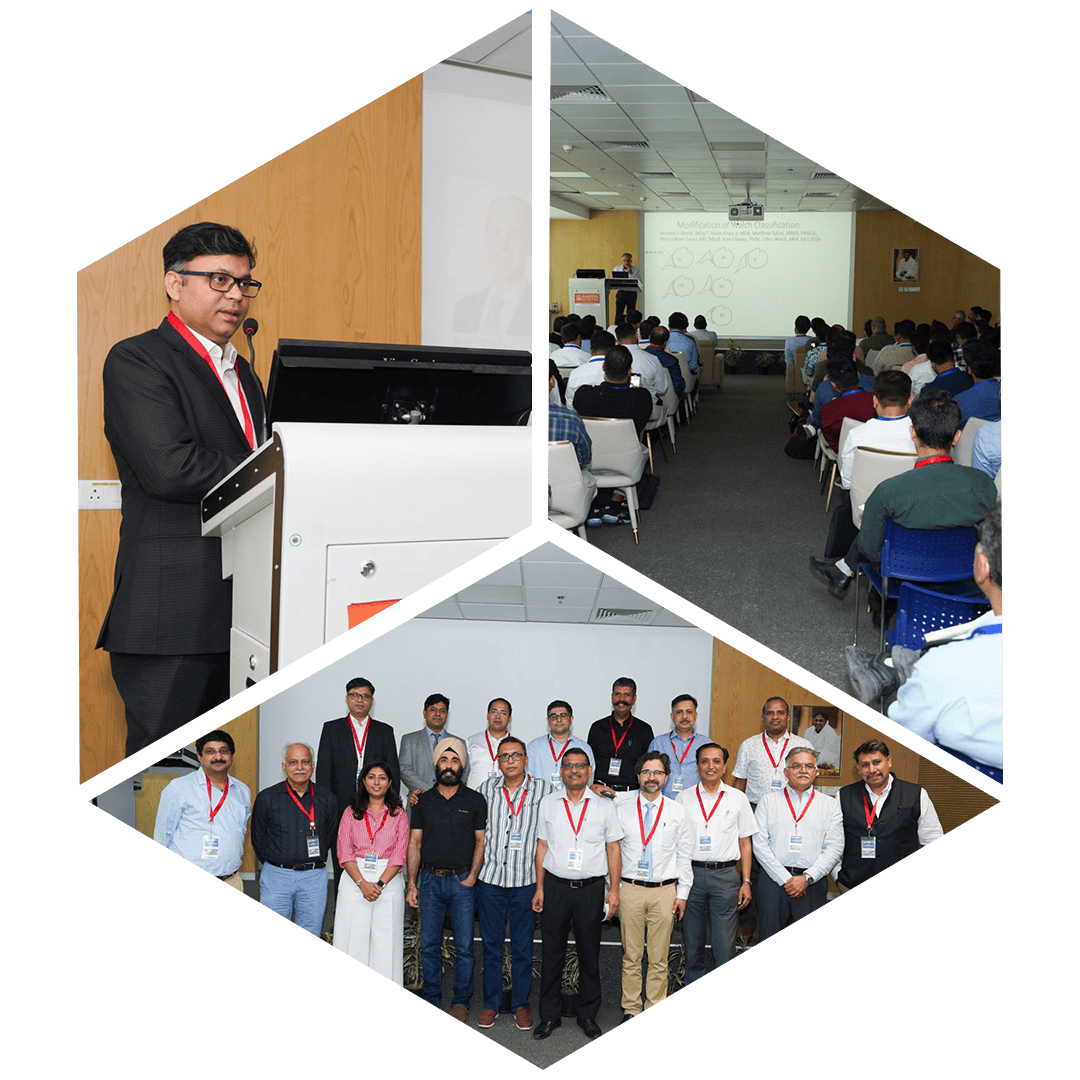
Delhi Shoulder Arthroplasty Course (DSAC)

DSAC was successfully organised on 19th May 2024 at Amrita hospital Faridabad under leadership of Dr Priyadarshi Amit. It was attended by over 150 orthopedic surgeons from all across the country. It was aimed at educating orthopedic surgeons about shoulder replacement procedures.
The next course DSAC - 2026 will be held on 7th - 8th August 2026 in New Delhi. This will be a two days event which will include Basic on the first day for beginners and Advanced course on second day for experienced surgeons.
More information to follow.
What People Speak About Us


Latest News