Shoulder dislocation surgery
Shoulder dislocation surgery is a medical procedure performed to stabilize the shoulder joint after it has been dislocated, particularly in cases of recurrent dislocations or when the initial injury results in significant damage to the joint structures. Below is a detailed explanation covering the anatomy, types of dislocations, indications for surgery, surgical procedures, recovery, risks, and outcomes.
The shoulder is a ball-and-socket joint, where the head of the humerus (upper arm bone) fits into the glenoid (a shallow socket in the scapula/shoulder blade). It’s the most mobile joint in the body, which also makes it more prone to instability.
Key stabilizing structures:
- Labrum – a fibrocartilage rim around the glenoid
- Capsule and ligaments – help hold the humeral head in place
- Rotator cuff muscles – provide dynamic support

Types of Shoulder Stabilization Surgeries
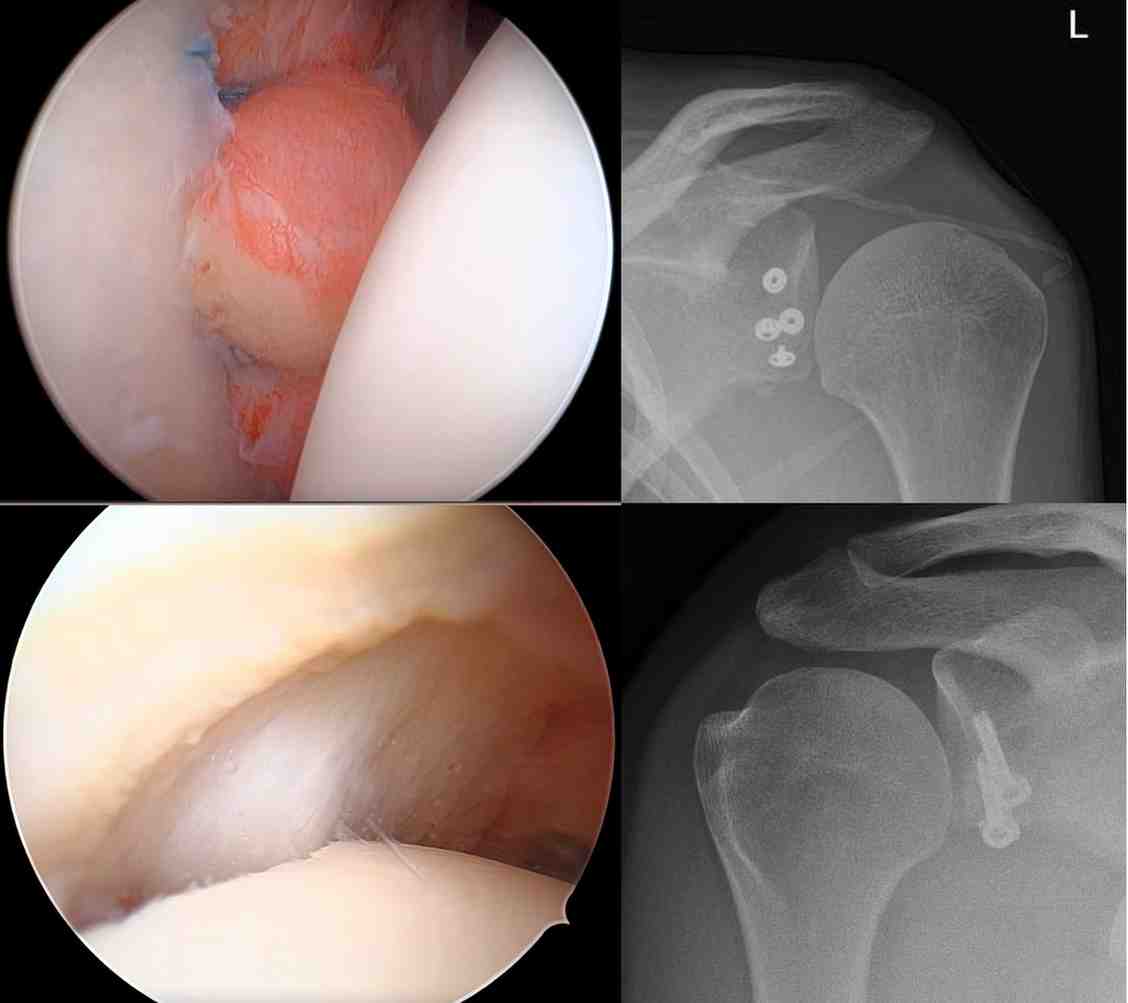
- Arthroscopic Bankart Repair
- Minimally invasive; performed using a camera (arthroscope) through small incisions
- The torn labrum and capsule are reattached to the glenoid rim using suture anchors
- Ideal for patients with soft tissue injury and minimal bone loss
- Latarjet Procedure
- Open surgery (can also be done arthroscopically by experienced surgeons)
- A portion of the coracoid process (a bony projection from the scapula) is transferred to the front of the glenoid
- Provides both bone support and a “sling effect” from the muscle attached to the coracoid
- Preferred for patients with significant bone loss or failed prior stabilization surgery
- Remplissage Procedure
- Performed in conjunction with Bankart repair
- Fills a Hill-Sachs defect (compression fracture of the humeral head) with the infraspinatus tendon
- Prevents engagement of the defect with the glenoid rim
- Capsular Shift or Plication
- Tightens the loose joint capsule
- Often combined with other procedures
Clinical Pathway
- You will be seen by the specialist in outpatient department for clinical evaluation.
- You will be asked certain questions related to your symptoms and examined thoroughly.
- Your investigations such as X-ray, MRI will be reviewed, following which a surgical plan of surgery will be made.
- A detailed explanation will be given to you with regards to surgery along with its pros and cons.
- You will be seen by the anesthetic team
- Your fitness for surgery will be evaluated.
- Investigations including blood tests will be carried out.
- A physical therapist will explain you with regarding to the post op precautions, exercises and immobilization.
- You will be admitted on the day of surgery in the morning. The surgery will be performed under general and regional anesthesia.
- After surgery, you will be under certain medication to control your post operative pain to make you comfortable.
- You will be discharged on the same or next day with post operative instructions.
- Your physical therapy will be started on the next day after surgery and will continue for around three months.
- You will be required to see the specialist in outpatient clinic on couple of occasions to assess the recovery. You were expected to recover completely in approximately three to six months.
If you’re considering or preparing for shoulder dislocation surgery, it’s crucial to:
- Discuss imaging results (MRI, CT) with your surgeon
- Understand the type of injury you have (labrum, bone loss, etc.)
- Commit to rehabilitation, as it’s as important as the surgery itself